Headaches aren’t just irritating—they can derail your entire day, mess with your productivity, and, if they’re chronic, significantly impact your overall well-being. Whether you’re a student cramming for finals, a busy parent juggling a million tasks, or someone stuck behind a desk all day, headaches don’t discriminate. The upside? Once you learn what type of headache you’re dealing with and what’s causing it, you can take control instead of letting it control you.
Let’s break it all down—from what headaches really are to how you can treat and prevent them.
So, What Is a Headache, Really?
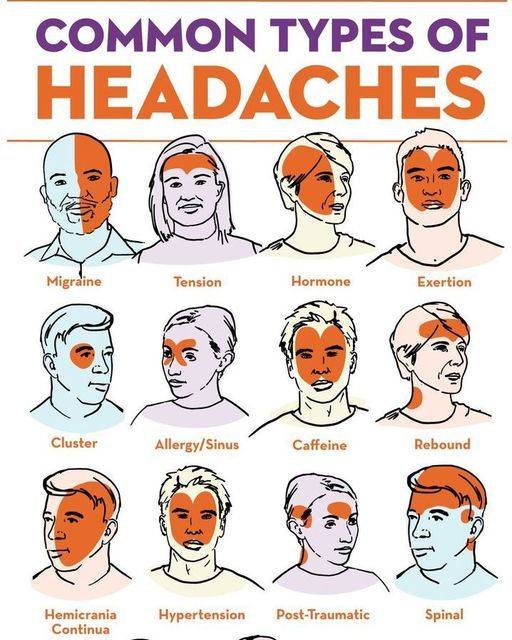
At its core, a headache is pain in the head—anywhere from a dull ache to sharp, pulsing pain. Most headaches fall into two main groups:
-
Primary headaches are conditions themselves—like migraines, tension headaches, or cluster headaches.
-
Secondary headaches are symptoms of something else going on, like sinus issues, hormonal changes, or dehydration.
Knowing which type you’re experiencing is the first key step toward finding real relief.
Primary Headaches: The Repeat Offenders
-
Migraines bring intense, sometimes incapacitating pain, often paired with nausea, light or sound sensitivity, and even visual auras. They can be triggered by hormonal shifts, stress, certain foods, and even weather patterns.
-
Tension headaches are the most common. They feel like a tight band is wrapped around your head, and they’re often linked to stress, sleep issues, or bad posture.
-
Cluster headaches are rare but brutally painful. They strike in groups or “clusters” and usually hit one side of the head near the eye, sometimes causing redness, watering, or a stuffy nose.
Secondary Headaches: Something Else Is Going On
-
Sinus headaches stem from inflammation or infection in the sinuses. Expect pressure around the eyes, cheeks, and forehead.
-
Hormonal headaches happen when estrogen levels fluctuate, often during periods, pregnancy, or menopause.
-
Medication-overuse headaches can sneak up on you. If you’re relying on pain meds too often, they might actually be the cause of recurring headaches.
Common Headache Triggers: What’s Setting You Off?
-
Stress and muscle tension: When stress hits, your muscles—especially around your neck and scalp—tense up. That tension can lead to headaches fast.
-
Hormonal changes: Estrogen dips and spikes play a major role in blood vessel behavior, which can trigger migraines.
-
Dehydration: Your brain needs water. When you don’t drink enough, it can slightly shrink, triggering pain.
-
Poor sleep: Inconsistent or insufficient sleep can mess with brain chemistry and increase inflammation, setting you up for a headache.
-
Certain foods: Skipping meals, overdoing caffeine, or consuming triggers like aged cheese, red wine, and processed meats can all contribute.
-
Sinus congestion: Allergies, colds, or even weather changes that inflame your sinuses can cause facial and head pain.
-
Eye strain: Too much screen time without breaks can stress your eyes and lead to headaches.
-
Weather shifts: Barometric pressure changes can affect fluid balance in your brain, especially for migraine sufferers.
-
Too many painkillers: Ironically, overusing medications like aspirin or ibuprofen can cause rebound headaches.
How to Treat Headaches the Smart Way
-
Over-the-counter meds like ibuprofen, acetaminophen, or aspirin are great for quick relief from tension headaches or mild migraines.
-
Prescription meds such as triptans or beta-blockers may be needed for chronic or severe migraines.
-
Stay hydrated—sometimes all your brain needs is water to bounce back.
-
Cold or hot compress: Use cold packs for migraines or warm compresses on your neck for tension headaches.
-
Massage therapy: Massaging your scalp, neck, or shoulders can help release tight muscles and ease pain.
-
Acupuncture has been shown to relieve chronic headaches by targeting pressure points.
-
Mind-body techniques: Breathing exercises, meditation, or progressive muscle relaxation can calm your nervous system and lower stress.
-
Sinus relief tools: Saline sprays, steam, or nasal steroids can ease sinus pressure.
-
Lifestyle fixes: Regular meals, better sleep habits, proper posture, and consistent exercise all add up to fewer headaches.
How to Prevent Headaches from the Get-Go
-
Drink more water: Aim for 8–10 glasses a day.
-
Stick to a sleep schedule: Aim for 7–9 hours and avoid late-night scrolling.
-
Check your posture: Especially if you sit at a desk—keep your back supported and screen at eye level.
-
Manage screen time: Use blue light filters and follow the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds).
-
Eat consistently: Don’t skip meals. Snack smart and limit sugar, caffeine, and alcohol.
-
Stress less: Take time to breathe, journal, stretch, or just get outside.
-
Get moving: Regular exercise releases endorphins, your body’s natural painkillers.
When to Call the Doctor
While many headaches can be handled at home, some require medical attention. See a doctor if:
-
The headache is sudden and severe
-
It comes with fever, confusion, vision changes, or trouble speaking
-
You’ve recently suffered a head injury
-
The headache keeps getting worse or won’t go away
Final Takeaway
Headaches are annoying, but they don’t have to rule your life. Whether they’re caused by stress, hormones, dehydration, or too much screen time, you can fight back. By identifying your triggers and making simple lifestyle changes, you’ll find yourself spending less time in pain and more time enjoying life. Your head deserves better—so start making small shifts today for a headache-free tomorrow.
-





